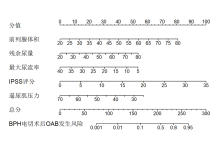
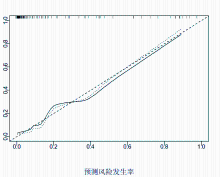
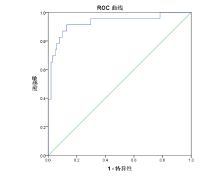
目的:建立良性前列腺增生(BPH)电切术后膀胱过度活动综合症(OAB)的列线图模型。方法:回顾分析2018年6月至2021年9月在我院行经尿道前列腺电切术的BPH患者124例,根据术后是否出现OAB分为OAB组23例和非OAB组101例。单因素及多因素Logistic回归分析BPH患者电切术后OAB的独立预测因素。R4.1.3软件构建列线图模型。结果:124例患者中23例术后出现OAB,发生率为18.55%。多因素Logistic回归分析结果显示前列腺体积、残余尿量、最大尿流率、IPSS评分、逼尿肌压力为BPH电切术后OAB发生的独立危险因素( P<0.05)。BPH电切术后OAB发生风险预测模型为:Y=0.072×前列腺体积+0.043×残余尿量-0.092×最大尿流率+0.131×IPSS评分-0.082×逼尿肌压力。采用R4.1.3软件构建列线图模型,Bootstrap法内部验证结果显示平均绝对误差为0.021,预测曲线与标准曲线基本拟合,提示模型预测准确度较高。ROC曲线下面积为0.929,95%CI为0.858~0.999,提示模型预测特异度高。结论:BPH电切术后OAB发生率较高,主要受前列腺体积、残余尿量、最大尿流率等因素影响,以上述因素构建的列线图模型具有较高的预测准确度。
Objective: To establish a nomogram model of over active bladder (OAB) after resection of benign prostatic hyperplasia (BPH).Methods: 124 patients with BPH who underwent transurethral resection of prostate in our hospital from June 2018 to September 2021 were retrospectively analyzed. They were divided into OAB group (n=23) and non-OAB group (n=101) according to whether OAB occurred after operation. Univariate and multivariate logistic regression were used to analyze the independent predictors of OAB in patients with BPH. R4.1.3 Software builds nomogram model.Results: OAB occurred in 23 of 124 patients, with an incidence rate of 18.55%. Multivariate logistic regression analysis showed that prostate volume, residual urine volume, maximum urinary flow rate, IPSS score and detrusor pressure were independent risk factors for OAB after BPH resection (P<0.05). The risk prediction model for OAB after BPH resection was: Y=0.072 ×prostate volume +0.043 ×residual urine volume –0.092 ×maximum urinary flow rate+ 0.131 ×IPSS score –0.082 ×detrusor pressure. The nomogram model is constructed by R4.1.3 software. The internal verification results of Bootstrap method showed that the average absolute error was 0.021, and the prediction curve was basically fitted with the standard curve, which indicated that the prediction accuracy of the model is high. The area under the ROC curve was 0.929, and the 95% CI was 0.858 to 0.999, indicating a high predictive specificity of the model.Conclusion: The incidence of OAB after BPH resection is high, which is mainly affected by prostate volume, residual urine volume, maximum urine flow rate and other factors. The nomogram model constructed by these factors has high prediction accuracy.
良性前列腺增生(benign prostatic hyperplasia, BPH)为中老年男性常见病, 主要以尿频、尿急、夜尿增加为表现, 该病不仅严重影响患者的正常生活, 还可能因尿潴留、输尿管返流而引起泌尿系统感染、肾功能破坏而对患者身体健康造成威胁[1, 2]。经尿道前列腺电切术为目前BPH的公认疗法, 该术式虽然疗效确切, 但术后仍有不少患者出现膀胱过度活动症 (over active bladder, OAB), 表现为尿急和尿失禁, 尿动力学检查为逼尿肌过度活动, 尿道-膀胱功能障碍等异常。OAB的发生不利于术后恢复, 需采取干预措施进行积极预防[3]。目前关于BPH电切术后OAB影响因素的研究虽有报道[4], 但并未以此建立预测模型, 对于临床指导价值有限, 本研究旨在通过建立BPH电切术后OAB发生的风险预测模型以预测OAB发生风险, 为干预人群的选择及干预措施的制订提供参考依据。
回顾分析2018年6月至2021年9月在我院行经尿道前列腺电切术的BPH患者124例, 年龄50~79(64.02±7.11)岁; 病程1~6(3.17±0.65)年; 术前国际前列腺症状评分(International Prostate Symptom Score , IPSS)5~27(17.02±3.18)分。根据术后是否出现OAB分为OAB组23例和非OAB组101例。纳入标准:(1)经影像学检查确诊为BPH, 并在我院行经尿道前列腺电切术; (2)术后无BPH症状且前列腺特异抗原(prostate specific antigen, PSA)<4μg/L; (3)拟分析的相关资料完整。排除标准:(1)术前膀胱容量<200ml; (2)术前有逼尿肌收缩无力表现者; (3)合并严重肝肾功能损伤者。
患者均由同一组医护人员进行手术, 腰麻成功后取膀胱截石位, 常规消毒铺巾, 经尿道置入电切镜后寻找精阜部位并以此为标志, 在膀胱颈部5、7点范围开始切除, 先修切前列腺中叶, 远端至精阜, 将多余腺体切除后以此为参照将左、右侧叶及12点位腺体进行切除, 深度达到前列腺薄膜, 最后对精阜部位前列腺组织进行修切, 修整前列腺创面使尖部圆整, 创面光滑。冲洗前列腺组织块后再次止血, 退镜, 留置三腔导尿管后气囊注水30ml, 以生理盐水持续冲洗膀胱至冲洗液颜色正常。
参考文献的基础上根据临床实践经验收集以下指标:(1)患者一般情况:年龄、BMI、合并疾病; (2)疾病相关指标:手术时间、前列腺体积、残余尿量、最大尿流率、平均尿流率、IPSS评分、逼尿肌压力、尿潴留情况[4, 5, 6]。
采用SPSS22.0统计软件对数据进行分析。计量资料符合正态分布用均数±标准差 ($\bar{x}±s$) 表示, 组间比较采用t检验。计数资料用例数(百分率)表示, 组间比较用χ2检验。单因素及多因素Logistic回归分析BPH患者电切术后OAB的独立预测因素。R4.1.3软件构建列线图模型。ROC曲线分析模型的预测价值。P<0.05为差异有统计学意义。
OAB组与非OAB组前列腺体积、残余尿量、最大尿流率、平均尿流率、IPSS评分、逼尿肌压力差异有统计学意义(P<0.05), 见表1。
| 表1 BPH电切术后OAB发生的单因素分析 |
以前列腺体积、残余尿量、最大尿流率、平均尿流率、IPSS评分、逼尿肌压力为协变量, OAB为因变量行多因素Logistic回归分析, 结果显示前列腺体积、残余尿量、最大尿流率、IPSS评分、逼尿肌压力为BPH电切术后OAB发生的独立危险因素(P<0.05), 见表2。
| 表2 BPH电切术后OAB发生的多因素Logistic回归分析 |
根据多因素分析中各因素B值构建BPH电切术后OAB发生风险预测模型, Prob=1/(1+e-Y), Y=0.072×前列腺体积+0.043×残余尿量-0.092×最大尿流率+0.131×IPSS评分-0.082×逼尿肌压力。因上述模型计算复杂, 为方便临床预测使用, 采用R4.1.3软件构建列线图模型, 结果见图1。
BPH为临床常见的男科疾病, 对于该病的治疗主要以手术切除病变组织为主, 但术后患者出现OAB的发生率较高。本研究124例患者中有23例术后出现OAB, 发生率为18.55%, 与过去的研究结果相一致[5]。
本研究多因素Logistic回归分析结果显示前列腺体积、残余尿量、最大尿流率、IPSS评分、逼尿肌压力为BPH电切术后OAB发生的独立性危险因素。分析原因:(1)前列腺体积方面:随着前列腺体积增加, 手术难度也相应增加, 操作过程中切除范围难以掌握, 术中大创伤的风险也越高, 且可能导致增生切除不完整而增加OAB风险[6, 7]。(2)残余尿量为BPH患者常用的病变程度判断指标, 主要用于逼尿肌损害及膀胱出口梗阻程度的判断。学界普遍认为当残余尿量达50~100ml时患者的逼尿肌即处于早期失代偿状态, 但当残余尿量>100ml时则可引起逼尿肌出现不可逆的损伤[8, 9]。(3)尿流率是单位时间内经尿道排出的尿量, 主要有最大尿流率、平均尿流率等指标, 其中最大尿流率意义最大, 主要用于下尿路梗阻的鉴别。当机体出现逼尿肌收缩力异常、膀胱出口梗阻时可致最大尿流率水平下降, 因而最大尿流率较低者OAB风险更高[10]。(4)IPSS评分在临床常用于反映BPH患者下尿路症状严重程度, 该评分实现了对排尿困难、尿频、尿急等BPH主观指标的客观评价。IPSS评分表中既包括了排尿等待、尿线变细、尿流中段等下尿路梗阻的相关问题, 也包含了尿急等膀胱刺激症状的内容, 可全面反映患者的逼尿肌功能[11]。本研究结果也显示IPSS评分为BPH电切术后OAB发生独立危险因素, 与上述观点一致。(5)逼尿肌压力改变是引起OAB的主要原因, 同时该指标也是判断膀胱逼尿肌功能状态及其受损程度的重要指标。在BPH治疗时应注意逼尿肌压力的改变, 对逼尿肌功能作出客观的评估, 尽量使逼尿肌功能处于可逆状态, 在代偿期及时进行治疗, 以保证逼尿肌功能的恢复[12]。
目前关于BPH电切术后OAB影响因素的研究虽有相关报道[13], 但均采用Logistic回归分析, 并未以此构建列线图模型。列线图模型为近年来逐渐在临床应用的预测临床事件概率的可视化模型, 该模型建立在Logistic回归模型的基础之上, 实现了Logistic回归模型的可视化, 计算方便、直观, 容易解释, 不仅可根据临床上影响疾病预后的多因素整合分析模型, 还可实现对患者个体化医疗的追求[14]。本研究在多因素分析的基础上建立了BPH电切术后OAB发生预测的列线图模型, 并经ROC曲线及Bootstrap法内部验证, 结果均显示本研究建立的模型具有较高的准确度与特异度。临床医护人员可在术前以此模型对患者各项目进行评分, 对于高风险患者可及时通过加强盆底肌肉训练、控制液体摄入、使用α 受体阻滞剂、术后镇痛等方式以降低患者术后OAB发生的风险, 以改善患者预后。
综上所述, BPH电切术后OAB发生率较高, 主要受前列腺体积、残余尿量、最大尿流率等因素的影响。以上述因素构建的列线图模型, 内部验证及外部验证结果均显示模型具有较高的预测准确度, 有助于协助临床一线医护人员及时识别高风险患者并提供合理的预防治疗决策。
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|