目的: 介绍保留Retzius间隙的机器人辅助腹腔镜前列腺癌根治术(RARP)的初步临床经验和疗效。方法: 分析2013年6月~2017年1月8例行保留Retzius间隙的RARP手术患者的资料。患者年龄56~71岁,中位年龄64岁,体质指数(BMI)19.7~24.1 kg/m2,中位数21.6 kg/m2。术前前列腺特异抗原(PSA)4.18~11.04 μg/L,平均7.50 μg/L。国际勃起功能指数(IIEF-5)≥21分6例,<21分2例。术前穿刺活检病理TNM分期T1c期4例,T2a期3例,T2b期1例。Gleason评分3+2=5分1例,3+3=6分7例。D'Amico风险分层均为低风险。手术使用4臂da Vinci Si手术系统,经腹腔建立操作通道。由Douglas腔上方的壁层腹膜切开,分离显露双侧输精管和精囊,悬吊提起双侧精囊,切开Denonvillier筋膜,分离前列腺后壁直至前列腺尖部,重新悬吊壁层腹膜,沿精囊前表面向前上方分离显露并离断膀胱颈部,筋膜内层面钝性分离前列腺前表面及两侧直至尖部,双连发钛夹处理离断前列腺侧蒂,最后离断前列腺尖部,将切除的前列腺置于标本袋内,由12点位开始双针逆时针方向连续吻合膀胱颈部及远端尿道残端。最后关闭Douglas腔前方的壁层腹膜。结果: 本组8例保留Retzius间隙的RARP手术均顺利完成。手术时间75~120 min,平均90 min。术中出血量50~200 ml,平均110 ml,均未输血。术后病理检查分期pT2a期5例,pTM2b期2例,pT2c期1例;1例手术切缘阳性,Gleason评分3+2=5分1例,3+3=6分6例,3+4=7分1例。术后拔除尿管时间14~21 d,平均17 d,拔管后控尿均满意,无尿失禁。术后住院天数4~7 d,平均5 d。术后随访4~41个月,平均14个月,无尿道狭窄,未观察到生化复发。术后3个月6例患者勃起功能满意,IIEF-5≥21分。结论: 保留Retzius间隙的RARP手术具有解剖合理性,对肿瘤根治疗效好,能有效保护血管神经束,术后性功能及尿控恢复满意。但仍需积累更多病例进行长期前瞻性的对照研究以证实其疗效。
Objective: To investigate the feasibility of the Retzius-sparing robot-assisted laparoscopic radical prostatectomy (RARP) and report the functional and oncologic results of our first 8 cases.Methods: From June 2013 to January 2017, 8 patients with clinically localized prostate cancer underwent this new approach for RARP. The patients were aged from 56 to 71 years old (mean 64), and the BMI was 19.7-24.1 kg/m2 (mean 21.6 kg/m2). The mean preoperative PSA was 7.50 (4.18-11.04) μg/L. Six patients had IIEF-5 ≥21, and 2 IIEF-5 <21. For the biopsy Gleason Score, 7 patients were scored 3+3=6, and the other 1 was scored 3+2=5. All of them were in a low D'Amico risk classification. The operation was performed using a 4 arm da Vinci Si operating system, and theworking channel was set up transperitoneally. The parietal peritoneum was incised at the anterior surface of the Douglas space. Seminal vesicles and deferens vasa were isolated and incised. Denonvillier's fascia was separated by the posterolateral surface of the prostate in an antegrade direction, reaching the prostatic apex, and then the bladder neck was isolated and dissected. The NVB was dissected using double interrupted titanium clips. The resected prostate was placed in a specimen bag after dissecting the prostatic apex. The anastomosis was performed using a continuous suture starting from the 12 o'clock position. The parietal peritoneum at the Douglas space level was finally closed.Results: All the operations were successfully performed. The total operative time was 75-120 min (mean 90 min). The blood loss was 50-200 mL (mean 110 mL) and no blood transfusion was required. Pathologic stage was pT2a in 5 patients, pT2b in 2 patients and pT2c in 1 patient, with positive surgical margin in one case. The postoperative pathologic Gleason score was 3+2=5 in 1 patient, 3+3=6 in 6 patients, and 3+4=7 in 1 patient. The catheter was removed after a mean of 17 (range: 14-21) days. No intra-operative complications occurred. The mean hospital stay was 5 (mean 4-7) days after surgery. All the cases were continent after removal of the catheter. No cases demonstrated vesicourethral stricture and biochemical recurrence during a postoperative follow-up period of 4-41 months. Three months after the operation, 6 patients had satisfactory erectile function (IIEF-5 ≥21).Conclusions: The Retzius-sparing RARP is oncologically safe and results in high early continence and potency rates. Long-term, prospective, comparative, and possibly randomized studies are needed.
根治性前列腺切除术是局限性前列腺癌的标准治疗方式, da Vinci手术系统于2000年获得美国FDA批准用于外科手术, 同年Binder和Abbou分别报道了机器人辅助腹腔镜前列腺癌根治术(robot-assisted laparoscopic radical prostatectomy, RARP)[1, 2], 此后10余年中RARP在前列腺癌高发的欧美国家迅速普及, 几乎取代了传统开放及腹腔镜手术, 其手术技术也不断发展, 如由Douglas腔先期到达精囊的Montsouris技术[3], 直接到达Retzius间隙的VIP(Vattikuti institute prostatectomy)技术[4]以及尿道膀胱吻合的Aalst技术[5]等。盆内筋膜, 血管神经束, 耻骨前列腺韧带, 阴部动脉以及Santorini血管丛是与术后保持性功能和尿控功能有关的解剖结构, 传统的RARP技术都是以既往开放耻骨后入路手术解剖为基础, 会对这些解剖结构造成损伤或存在损伤风险, 进而存在引起术后性功能和尿控功能异常的风险。因此意大利Aldo Bocciardi教授团队提出保留Retzius间隙经由前列腺底部平面行RARP的Bocciardi技术[6]能够有效避免术中这些解剖结构的损伤, 并取得良好的肿瘤控制和术后功能恢复的效果[7]。2013年我中心在国内首次成功完成1例保留Retzius间隙的RARP手术。现将2013年6月~2017年1月行保留Retzius间隙的RARP手术病例报告如下。
2013年6月~2017年1月我中心行保留Retzius间隙的RARP 8例, 年龄56~71岁, 中位年龄64岁。体质指数(body massindex, BMI)19.7~24.1 kg/m2, 中位数21.6 kg/m2。术前PSA 4.18~11.04 μ g/L, 平均7.50 μ g/L。国际勃起功能指数(International Index of Erectile Function-5, IIEF-5)≥ 21分6例, < 21分2例。术前穿刺活检病理TNM分期T1c期4例, T2a期3例, T2b期1例。Gleason评分3+2=5分1例, 3+3=6分7例。D'Amico风险分层均为低风险。
1.2.1 机器人手术系统的建立 全麻成功后取半截石位用Allen脚蹬固定下肢。消毒术野皮肤, 铺无菌巾单。经脐内边缘3 mm切口穿刺置入Veress气腹针建立气腹, 于脐正中上方两横指处纵行切开10 mm切口, 随后插入12 mm套管, 作为机器人镜头通道。置入镜头, 直视下放置其他套管。两个8 mm套管分别置于脐水平距脐约8~10 cm位置, 左侧为2号操作臂通道, 右侧为1号操作臂通道。第3个8 mm套管置于右侧1号操作臂通道外侧8~10 cm处, 作为3号操作臂通道。于2号操作臂通道外上方8~10 cm处平镜头通道水平放置12 mm套管作为助手通道。此后患者取35~45° 的Trendelenburg体位, 机器人以脐正中线为轴向患者分开的两腿间移动。连接镜头臂和3个操作臂。将30° 向下镜头安装于镜头通道, 1号操作臂安装单极弯剪, 2号操作臂安装双极Maryland钳, 3号操作臂安装Prograsp抓钳, 助手位于患者左侧。
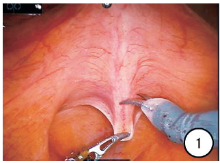
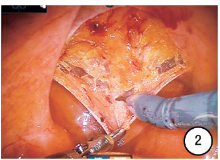
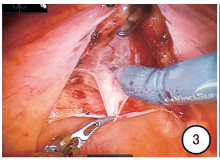
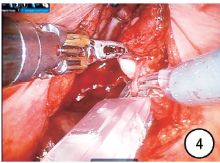
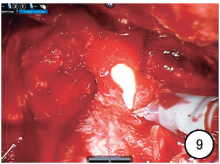
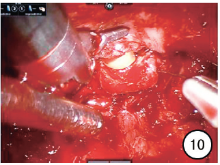
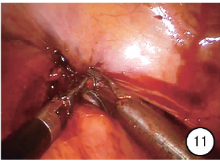
1.2.2 手术步骤 先游离左侧乙状结肠, 将其向腹侧牵拉, 显露Douglas腔, 切开Douglas腔上方壁层腹膜5~7 cm (图1, 2), 分离显露双侧输精管和精囊(图3, 4), 以荷包缝线悬吊向腹壁提起双侧精囊(图5), 沿精囊根部前列腺侧后方并沿筋膜内层面向前推开分离Denonvillier筋膜, 沿此平面用双连发钛夹分段结扎前列腺侧韧带, 钝性与锐性结合分离, 直至前列腺尖部(图6, 7), 于筋膜内保留阴茎勃起神经, 松开悬吊的精囊, 重新向腹壁悬吊前述切开的壁层腹膜上缘, 显露并离断膀胱颈部(图8), 钝性分离前列腺前表面直至尖部, 离断前列腺尖部尿道(图9), 将切除的前列腺置于标本袋内, 由12点位开始双针逆时针连续吻合膀胱颈部及远端尿道残端(图10)。最后关闭Douglas腔前方的壁层腹膜(图11)。于Douglas腔留置盆腔引流管, 取出标本, 观察大体标本包膜是否完整(图12), 缝合各切口, 手术结束。
8例手术均成功完成, 无一例中转开放手术。手术时间75~120 min, 平均90 min。术中估计失血量50~200 ml, 平均110 ml, 均未输血。术后病理检查均为前列腺腺癌, Gleason评分3+2=5分1例, 3+3=6分6例, 3+4=7分1例, 病理分期pT2a期5例, pT2b期2例, pT2c期1例, 1例手术切缘阳性。术后住院4~7 d, 平均5 d, 于术后3~4 d(平均3.3 d)拔除盆腔引流管, 无术后吻合口漏尿发生。术后14~21 d拔除尿管, 平均17 d, 拔管后均尿控满意, 无尿失禁。术后随访4~41个月, 平均14个月, 无尿道狭窄, 复查PSA均< 0.06 μ g/L, 未观察到生化复发。术后3个月6例患者勃起功能满意, IIEF-5≥ 21分。
为了保护与性功能及排尿功能相关的解剖结构, 2010年意大利Aldo Bocciardi教授团队提出了保留Retzius间隙的RARP手术入路[6]。据其报道, 68.8%的患者术后取得“ 三连胜” 结果(满意的尿控和勃起功能, 1年无生化复发)[7]。
2013年开始我中心在国内率先实践了这种手术入路, 根据我们的体会, 同传统的RARP手术入路相比, 该术式具有以下优点:①这种入路能够完全在筋膜内切除前列腺, 充分保留血管神经束的完整性, 达到保护术后患者性功能的目的, 另外一些报道指出前列腺除了5点和7点位的血管神经束外, 其周围还有很多血管及神经纤维[8], 尸体解剖发现这些血管及神经同时供应和支配着尿道外括约肌和阴茎海绵体[9], 该入路能够完整保留盆底筋膜, 避免了对前列腺周围这些血管及神经的损伤; ②该入路可以避开前列腺前面的Santorini血管丛, 减少术中出血, 另外, Santorini血管丛中含有一些细小动脉, 这些小血管可能部分供应尿道外括约肌或者阴茎海绵体, 保护好这些血管对远期性功能和尿控功能的恢复具有积极意义; ③保留了耻骨前列腺韧带及阴部动脉的完整性, 已有研究报道保护这些结构能使患者术后尿控功能和性功能获益[10]; ④传统入路的RARP需要呈倒U型完全打开膀胱前表面的Retzius间隙, 而该术式无需打开Retzius间隙, 仅在Douglas腔的5~7 cm切口内完成手术, 相较传统入路更为微创化。本组8例患者, 2~3周拔除尿管后均无尿失禁发生, 术前6例 IIEF-5≥ 21分的患者, 其术后3个月时IIEF-5仍≥ 21, 性功能恢复满意。术后盆腔留置引流管平均3.3 d即拔除, 无漏尿发生, 这些应归功于该术式的微创化及对前列腺周围术后功能相关解剖结构的充分保护。
保留Retzius间隙的RARP的主要技术难点有:①操作空间狭小, 前列腺体积越大操作空间越狭小, 若再合并腺体周围粘连, 则组织分离更加困难, 为尽可能显露术区需要排空膀胱并充分提拉膀胱后壁; ②膀胱尿道吻合, 因前列腺周围筋膜结构术中未行分离, 在行膀胱颈部和尿道吻合时存在张力, 而且吻合操作为自下而上的反向视野, 需要一定的吻合技巧, 此时可更换0° 或30° 向上镜头, 并采用带倒钩的V-LocTM缝线, 自12点位双针逆时针连续减张缝合, 前壁吻合完成后, 适当用力收紧缝线, 使膀胱尿道吻合口前壁完全靠拢, 插入尿管, 继续连续缝合吻合口后壁, 最后在12点位线尾打结。③由于该术式是完全筋膜内切除, 对于中高危, 尤其高危的前列腺癌, 是否会增加切缘阳性的风险, 需要进一步观察。本组病例中有1例切缘阳性, 因此应严格把握手术指征。
综上所述, 保留Retzius间隙的RARP治疗局限性前列腺癌在技术上是可行的, 术中能够完整的保护与性功能及尿控功能相关的前列腺周围的解剖结构。尤其适合对尿控及勃起功能要求高、小体积、早期的前列腺癌。从肿瘤控制角度及适应证范围, 该术式能够大规模推广, 还需要更多病例做长期的随访及与传统入路对比分析。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|